Introduction
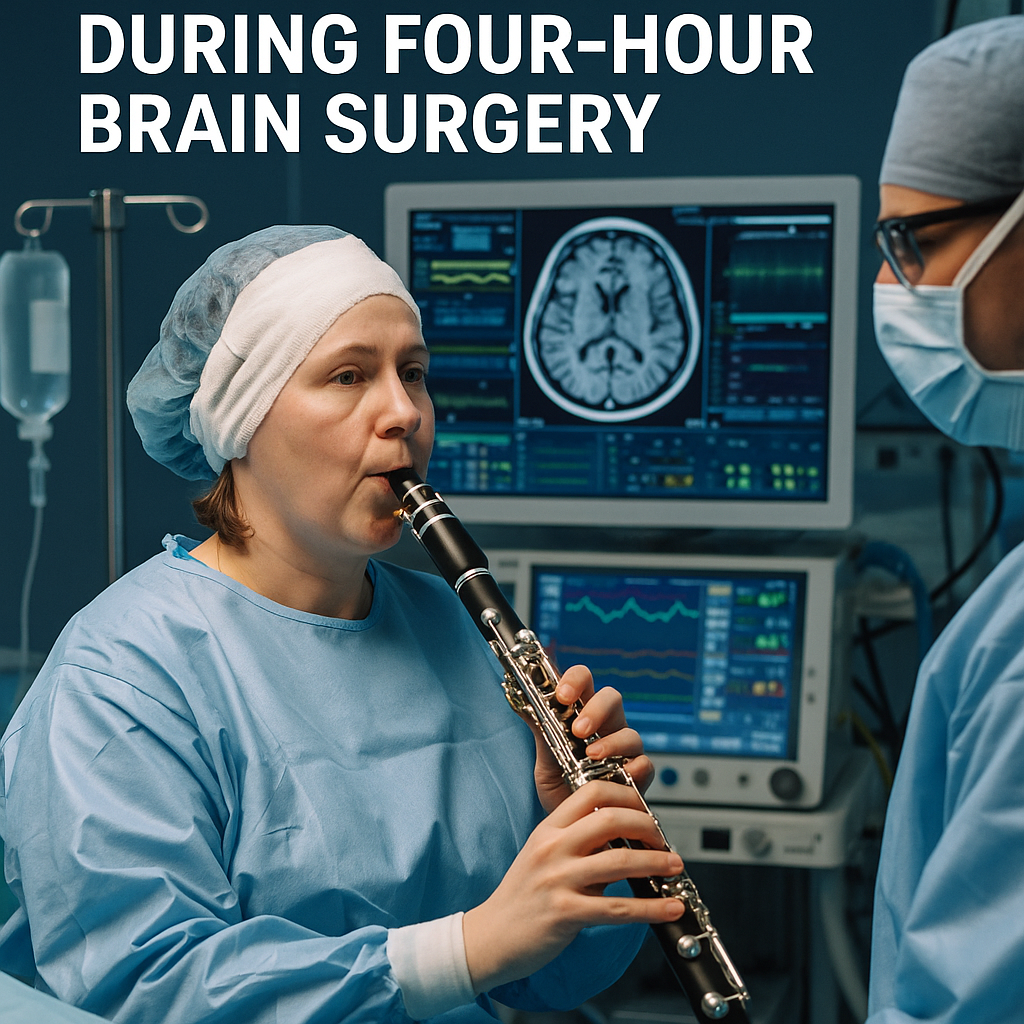
A woman with Parkinson’s disease played the clarinet while awake during a four-hour brain operation to help surgeons map critical regions and preserve motor and auditory functions. The procedure, an example of awake craniotomy and intraoperative functional mapping, highlights not only advances in neurosurgery but also accelerating intersections between neurotechnology, AI, data security and the startup ecosystem that funds and commercializes these innovations.
Body
Awake brain surgery is a well-established technique for surgeries near eloquent areas of the brain. Patients remain awake so surgeons can stimulate and monitor brain regions in real time, ensuring that speech, movement and other functions are avoided during resection or electrode placement. In this case, having the patient play a wind instrument provided an exceptionally granular, task-specific readout of motor control, breath regulation and auditory feedback while surgeons intervened.
From a technology perspective, the operation benefited from modern neuronavigation, cortical stimulation mapping and intraoperative imaging. Increasingly, teams layer these techniques with AI-driven signal analysis. Machine learning algorithms can parse local field potentials and cortical responses faster than human interpretation alone, flagging patterns that indicate risk to speech or fine motor control. AI models trained on multimodal surgical data are beginning to assist in surgical planning, electrode targeting for deep brain stimulation (DBS) and in predicting postoperative outcomes.
The surge in interest and funding for neurotech startups is directly relevant. Companies developing closed-loop DBS, noninvasive neuromodulation, implantable sensors and analytics platforms have attracted venture capital and strategic investment. Investors cite aging populations and the clinical need for Parkinson’s therapies as drivers. Startups are also integrating music and task-based paradigms into clinical platforms because real-world, task-specific biomarkers — like playing a clarinet — can be more sensitive to change than standard motor scales.
Data management and security have become focal points as surgical and chronic neuro-monitoring data scales up. Blockchain and distributed ledger technologies are being explored to provide immutable audit trails for consent, device provenance and patient-generated data, improving traceability across care teams and research consortia. While blockchain won’t replace HIPAA-compliant storage, it can augment interoperability and consent management in multi-center studies that feed AI models.
Geopolitically, the race to lead in neurotechnology spans universities, startups and national labs across North America, Europe and Asia. Governments are launching funding initiatives and regulatory frameworks to accelerate safe commercialization. That creates opportunities for cross-border partnerships but also scrutiny around export controls, supply chains for specialized semiconductors and ethical standards for neural data. Startups seeking growth should weigh geopolitical risk in supply procurement and clinical trials.
Ethical and business considerations converge in the operating theater. Real-time patient participation—playing an instrument—underscores patient autonomy and offers compelling clinical value. For investors and entrepreneurs, successful demonstrations like this help de-risk product concepts and make clinical endpoints more tangible to regulators and payers.
Conclusion
This case of a musician playing clarinet during a four-hour awake surgery is more than a remarkable human-interest story; it exemplifies how clinical practice, AI analytics, secure data infrastructure and startup innovation are converging to reshape care for neurological diseases. As neurotech startups continue to attract funding, and as regulators adapt, expect more integrations of task-based biomarkers, AI-supported intraoperative decision tools and distributed data solutions. The combination of patient-centered techniques and emerging technologies promises improved outcomes for Parkinson’s patients, but also raises important questions around privacy, cross-border collaboration and equitable access.